Abstract
Background: CD19-targeting chimeric antigen receptor (CAR) T-cell therapy has shown great efficacy in patients with refractory/relapsed non-Hodgkin lymphoma (NHL), but was associated with serious adverse effects such as cytokine release syndrome (CRS). It has been speculated that NHL baseline disease burden might affect clinical outcome and CRS, but such assumption has not been explored in detail in previous studies. Metabolic tumor volume (MTV) and total lesion glycolysis (TLG), calculated using FDG PET-CT, are quantitative indicators of baseline tumor burden.
Methods: Utilizing FDG PET-CT, we calculated MTV and TLG at baseline and post CAR T-cell therapy in 15 patients with NHL.
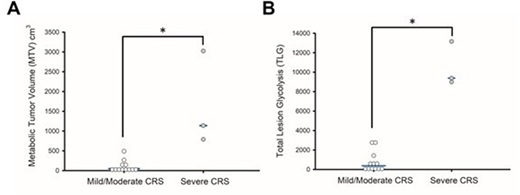
Results: Among all the patients, the median MTV was 72 (range 0.02-3024.9) cm3 and the median TLG was 610.1 (range 0.011-13156.3). After a median follow-up of 6 months, the overall response rate (ORR) was 66.7% (95% CI 38.4-88.2%). The baseline MTV and TLG did not have significant difference in patients with or without response (p=0.271 and 0.95, respectively). Cox-regression analysis did not find lower baseline MTV and TLG significantly associated with better overall survival (p=0.67 and 0.45, respectively). Patients with mild and moderate CRS (defined as Grade 0-2) had significantly lower MTV and TLG than those with severe CRS (Grade 3, 4) (median MTV: 49.3 v.s. 1137.7 cm3, p=0.012; median TLG: 379.1 v.s. 9384, p=0.012, Figure A, B). The median MTV in patients received tocilizumab, an IL-6 antagonist for the treatment of severe CRS, was 963.4 cm3, which was significantly higher than the patients not receiving tocilizumab (58.1 cm3, p=0.037). The median TLG in patients received tocilizumab was 9187.1, compared with 610.1 in patients not receiving tocilizumab (p=0.053). Using FDG PET-CT, we also demonstrated that CAR T-cell therapy in NHL patients could associate with severe local complications such as local compression and local inflammation.
Conclusions: Low NHL baseline disease burden is not associated with better response rate or long-term outcome. Patients with higher baseline disease burden have more severe CRS
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal